Retinopathy of Prematurity
What is retinopathy of prematurity?
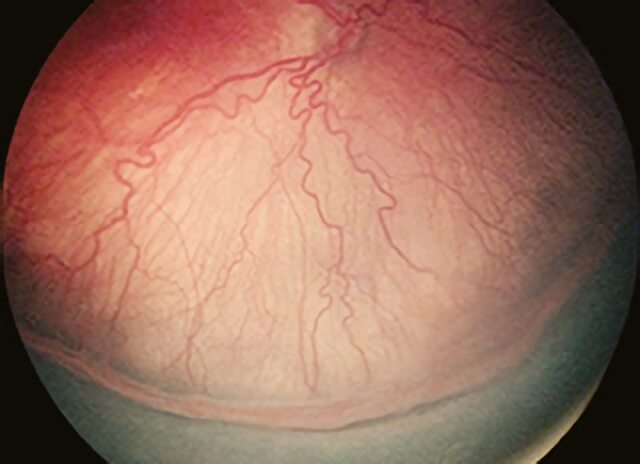
Retinopathy of prematurity is a condition affecting premature infants of low birthweight (BW) and young gestational age (GA). It occurs when the development of normal retinal blood vessels, which typically requires a full-term pregnancy for completion, is interrupted by the premature birth. If the disease progresses, scar tissue can grow; this can lead to retinal detachment and vision loss.
Though great strides have been made in the care of profoundly premature infants and survival rates have improved considerably, retinopathy of prematurity remains a leading cause of lifelong visual impairment. Retinopathy of prematurity causes visual loss in 1300 children and severe visual impairment in another 500 children each year in the United States alone.
More mildly affected infants may experience moderate vision loss and crossed eyes.
Learn more about retinopathy of prematurity at ASRS
What is the prognosis for infants with retinopathy of prematurity?
In 85% to 90% of cases, retinopathy of prematurity of milder severity resolves on its own, with no meaningful impact on vision. If retinopathy of prematurity progresses to an advanced stage, an infant may:
- Not respond appropriately to light
- Have white scar tissue visible in the pupils
- Develop an oscillating (back and forth) involuntary eye movement (nystagmus, pronounced nis TAG mus) by as early as 3 months after the original scheduled date of birth
- Progress to blindness
What are the causes of retinopathy of prematurity?
The earliest cases of retinopathy of prematurity were thought to be the result of introducing oxygen therapy into the newborn nursery to improve the survival rates of premature infants. Though more premature infants survived, some progressed to blindness. In 1942, oxygen was identified as an agent that could aggravate this process and lead to retinal detachment. Today, the use of oxygen is closely monitored and is no longer implicated as the sole or even a primary factor in retinopathy of prematurity development. While the survival rate for high-risk newborn infants has improved, the incidence of retinopathy of prematurity has remained constant since the mid-1990s.
What are the risk factors for retinopathy of prematurity?
Retinopathy of prematurity is a disease of the smallest and the sickest infants. Premature birth and low birthweight are the primary risk factors. Other risk factors for the development of retinopathy of prematurity include:
- Multiple births
- Other health problems involving the lungs and intestines
- Infection
How is retinopathy of prematurity diagnosed?
Infants of low birthweight (under 1500 grams or 3.3 lbs.) and gestational age (30 weeks or less)—as well as infants deemed higher risk by the neonatologist (due to multiple births, oxygen exposure after birth, etc.)— are screened with either bedside eye exams or digital pictures of the back of the eye (retina), which are then reviewed by a physician experienced in the diagnosis and treatment of retinopathy of prematurity. Once retinopathy of prematurity progresses to a certain level of severity, treatment is recommended. Treatment is most often required between 34 to 38 weeks of gestation.
How is retinopathy of prematurity treated?
Since the early 1990s, retinopathy of prematurity has been successfully treated in most infants by placing laser burns in the part of the retina that has not developed normal blood vessels1. This approach prevents retinal detachment in 90% of treated eyes with few long-term side effects. Since 2007, injection of certain drugs (bevacizumab [Avastin®] or ranibizumab [Lucentis®]) into the eye to suppress growth of the abnormal blood vessels has been employed by some physicians2.
To date, dosing and long-term safety information are lacking, and laser is generally the preferred approach to managing retinopathy of prematurity requiring treatment, except for those very small babies with very aggressive retinopathy of prematurity. If an eye goes on to develop retinal detachment, surgery may be performed to help reattach the retina, but the goal is to try to screen in order to treat retinopathy of prematurity at the right time to stop the progression to retinal detachment.
Once retinopathy of prematurity progresses to a certain level of severity, treatment is recommended.
References
- Houston SK, Wykoff CC, Berrocal AM, Hess DJ, Murray TG. Laser treatment for retinopathy of prematurity. Lasers Med Sci. 2013 Feb;28(2):683-92. https://pubmed.ncbi.nlm.nih.gov/22134790/
- Wykoff CC,Houston SK, Berrocal AM. Anti-Vascular Endothelial Growth Factor Agents for Pediatric Retinal Diseases, International Ophthalmology Clinics. Winter 2011; 151(1):185-199. https://journals.lww.com/internat-ophthalmology/Citation/2011/05110/Anti_Vascular_Endothelial_Growth_Factor_Agents_for.11.aspx
+Information and images for retinopathy of prematurity is from the American Society of Retina Specialists
+Copyright 2016 The Foundation of the American Society of Retina Specialists. All rights reserved.
Schedule Retinopathy of Prematurity Treatment in Northern California with Retinal Consultants Medical Group
Since 1975, Retinal Consultants Medical Group has been providing outstanding care to patients throughout Northern California, including Sacramento, Modesto, and Stockton. Our retina specialists and surgeons treat multiple vitreoretinal conditions, such as age-related macular degeneration and diabetic retinopathy. We invite you to contact us with any questions or schedule an appointment today.


