Nonproliferative Diabetic Retinopathy
What is nonproliferative diabetic retinopathy?
High blood sugar levels cause damage to the fine vessels that supply blood to the retina, the light-sensitive tissue inside your eyes. As this damage accumulates, your doctor can begin to see the earliest signs of diabetic changes in your retina – distortion of the vessels and tiny retinal hemorrhages. When the damage has not progressed to the point where new, abnormal blood vessels are growing to try to replace damaged ones, then we call the diabetic damage “nonproliferative diabetic retinopathy.”

This color photograph illustrates areas of red dots and blots that indicate hemorrhage from diabetic damage to the retina. Also, there are white areas of fatty deposition in an area of swollen retina, a condition called diabetic macular edema
Learn more about Nonproliferative Diabetic Retinopathy
My vision seems fine. Can I still have diabetic retinopathy?
Yes. Often there are no visual symptoms in the early stages of nonproliferative diabetic retinopathy. The vision usually deteriorates as progressive damage occurs to the vessels in the central part of the retina, called the macula. Diabetic injury to the blood vessels in the macula can cause swelling (diabetic macular edema) or ischemia – nerve damage from lack of blood flow. It is important not to wait for symptoms to occur before having your eyes examined for diabetic damage. Treatments to preserve your vision from diabetic damage are much more successful if the disease is consistently monitored and treated in its earlier stages
How is the diagnosis of nonproliferative diabetic retinopathy made?
The first step is a careful eye exam where both pupils are dilated. To supplement the direct examination of your eye with lights and lenses, the circulation of the retina can be carefully assessed with a special test called a fluorescein angiogram. This is a photographic study of the back of the eye performed after an orange-colored dye is injected in a vein in the hand or arm. The dye circulates through the body into the eye to highlight abnormal vessels, or where treatment may be needed. In addition, the degree and extent of damage to the center of the retina, called the macula, can be evaluated by a painless retina imaging system called an optical coherence tomography scan (OCT).
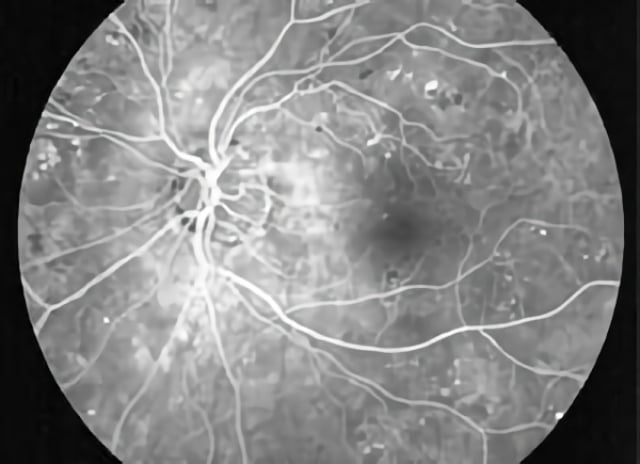
This is an example of an angiographic image of nonproliferative diabetic retinopathy. Note the dark spots indicating areas of hemorrhage and the white dots that indicate areas where diabetes has damaged blood vessels.
How is nonproliferative diabetic retinopathy treated?
Not all forms of nonproliferative diabetic retinopathy require treatment to the eyes, but all patients require continued care and blood sugar control through their primary care provider. If the diabetic damage includes a significant degree of swelling in the central portion of the retina, a condition called diabetic macular edema, medical therapy with injections of drugs in the eye or laser therapy may be recommended for the eyes involved. Injections of medications have become the most common modern treatment for diabetic macular edema and have the greatest chance for arresting the progression of the diabetic damage and in some cases restoring some lost vision. (See Diabetic Macular Edema.) Laser photocoagulation is also a common treatment for nonproliferative diabetic retinopathy with macular edema. In this kind of procedure, painless brief spots of bright light are used to treat the retina to reduce further loss of vision from diabetic macular edema. Laser surgery may need to be repeated several times. If the diabetic retinopathy progresses beyond the nonproliferative stage to the proliferative stage, a different type of laser therapy may be recommended. (See Proliferative Diabetic Retinopathy.)
Schedule Nonproliferative Diabetic Retinopathy Treatment in Northern California with Retinal Consultants Medical Group
Since 1975, Retinal Consultants Medical Group has been providing outstanding care to patients throughout Northern California, including Sacramento, Modesto, and Stockton. Our retina specialists and surgeons treat multiple vitreoretinal conditions, such as age-related macular degeneration and diabetic retinopathy. We invite you to contact us with any questions or schedule an appointment today.


