Diabetic Macular Edema
What is diabetic macular edema (DME)?
The retina lines the back wall of the eye. It is responsible for receiving light from the outside world and sending the light image to the brain. The retina needs nutrients and oxygen to survive, which it receives through an extensive network of small blood vessels. These small blood vessels are at risk for damage from high blood sugar – as occurs in diabetes. When these vessels are damaged they can shut down entirely or become leaky. When the blood vessels leak, the normally dry retina soaks up the fluid like a sponge, causing the retina to thicken. When this thickening occurs in the center of the retina – the macula – it is called diabetic macular edema.
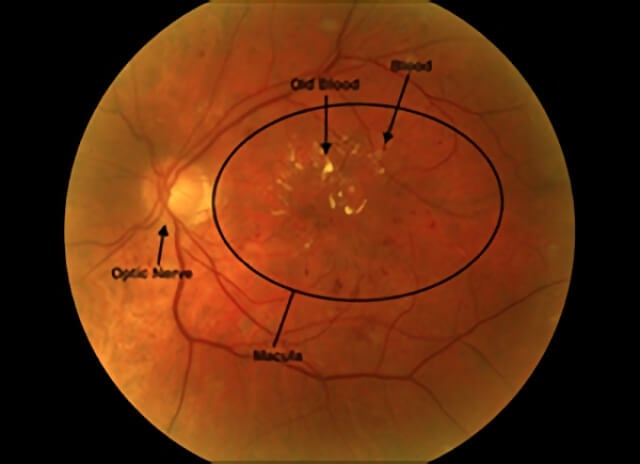
A color photograph of a diabetic patient’s retina, showing a collection of old blood that has leaked into the macula from damaged blood vessels.
Who is at risk for having diabetic macular edema?
All patients with diabetes are at risk. High blood pressure and high cholesterol are additional risk factors.
How is diabetic macular edema diagnosed?
Usually patients report blurry vision in one or both eyes over several months. These patients often report a history of diabetes control that has not been optimized. Examination of the retina with specialized lights and lenses after dilation of the pupils can discover signs of diabetic macular edema. Computerized photographic tests such as a fluorescein angiogram (FA) and optical coherence tomography (OCT) help us find which blood vessels are damaged and determine how much fluid has leaked into the retina. An FA is done by injecting an orange dye into a vein of the arm and taking special digital photographs of the dye as it flows through the blood vessels in the retina to look for abnormalities. An OCT is a painless computerized scan of the retina that provides a detailed view of the inner retinal structures.
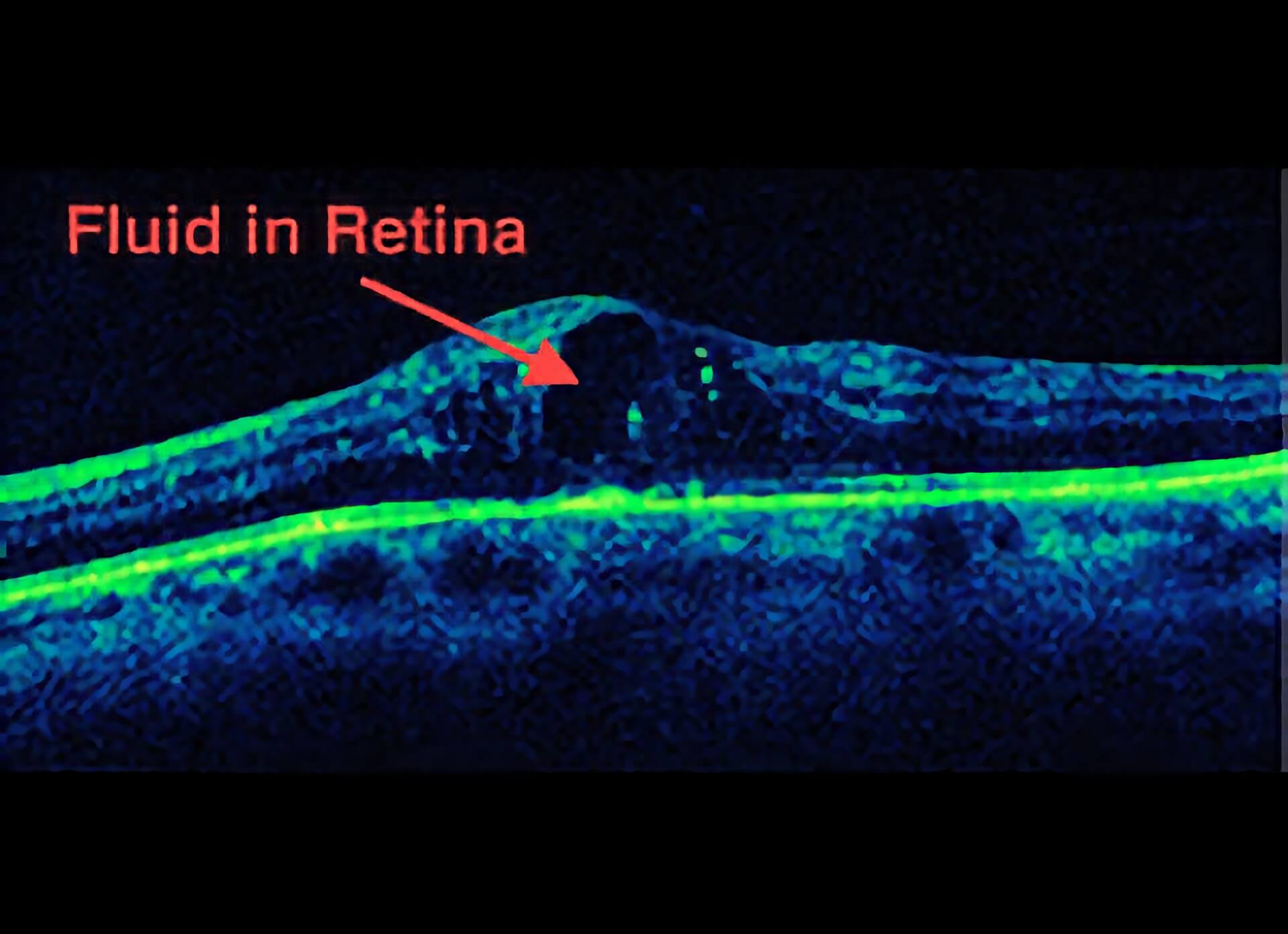
An OCT photo showing a high resolution slice through the macula of a diabetic patient. The black spot represents fluid that has leaked into the macula
What can be done for diabetic macular edema?
The backbone of all treatments for diabetic macular edema is good blood sugar and blood pressure control. In patients who need immediate help while they work on their systemic health issues, there are several treatment options that may help. Laser can be applied to areas of damaged blood vessels and damaged retina to help reduce leaking and assist in fluid reabsorption. For vision that is reduced because of fluid accumulation, anti-VEGF and steroid medications can be used to help fluid reabsorb. Anti-VEGF medications were developed to remove VEGF (Vascular Endothelial Growth Factor), a major factor in making blood vessels leaky. These medications must be delivered as an injection in the eye after anesthetic and antiseptic treatment to the eye to make the injection as comfortable and safe as possible. Since the introduction of anti-VEGF medications, many clinical trials have proven their efficacy1 (Ou et al. 2017). Bevacizumab (Avastin), Ranibizumab (Lucentis), and Aflibercept (Eylea) are the most useful anti-VEGF drugs we have available today.
In addition to anti-VEGF medications, steroids have been found in randomized clinical trials to be another tool to help combat DME. Steroids help damaged blood vessels heal properly by addressing the inflammatory component of DME. A long acting dexamethasone steroid implant (Ozurdex) has been shown in the MEAD study to improve vision for DME. The laser, Anti-VEGF and steroids address DME in different ways and your retinal consultant will help decide which treatment regimen is right for you
How frequently do I need Injections?
The anti-VEGF agents currently available last for 4-6 weeks before their effects fade and a new injection is typically needed. Most clinical trials show that treatment every 4-8 weeks gives the best results. The steroid implants may last even longer and retreatment may not be needed for several months. Some patients need more frequent injections and others need less frequent injections. The intervals required by any one patient may change with time. Your doctor will decide with you how frequently you need treatment.
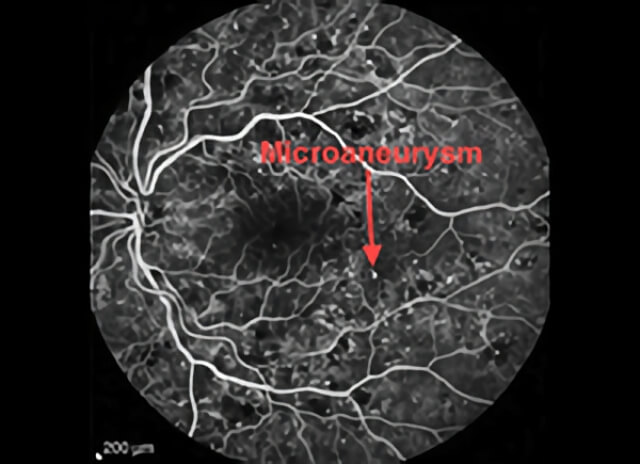
A fluorescein angiography photo of a diabetic patient’s retina. All the small white spots are sites of damage to blood vessels called microaneurysms. Microaneurysms often leak fluid.
Does the injection hurt?
The procedure is quick and practically pain free for most patients. A sterile lid speculum helps keep the eye open and an antiseptic kills germs that may cause an infection. It is common for the eye to feel irritated and scratchy for a day after the injection. Worsening vision and severe pain, especially if it is not improving after the first day may be signs of an infection after an eye injection and if you have these symptoms you must contact your doctor.
Will I go blind from diabetic macular edema?
Diabetic macular edema is one part of a larger problem, diabetic retinopathy, so there is a wide range in visual outcomes for patients with Diabetic Macular Edema. The final visual outcome cannot be predicted. In general, the faster we identify and treat the problem, the better. Encouraging clinical trial results suggest that with treatment less than 4% of patients will go blind after 3 years.
References
- Ou WC, Brown DM, Payne JF, Wykoff CC. Relationship Between Visual Acuity and Retinal Thickness During Anti-Vascular Endothelial Growth Factor Therapy for Retinal Diseases. Am J Ophthalmol. 2017 Aug;180:8-17. pubmed.ncbi.nlm.nih.gov/28549848
Schedule Diabetic Macular Edema Treatment in Northern California with Retinal Consultants Medical Group
Since 1975, Retinal Consultants Medical Group has been providing outstanding care to patients throughout Northern California, including Sacramento, Modesto, and Stockton. Our retina specialists and surgeons treat multiple vitreoretinal conditions, such as age-related macular degeneration and diabetic retinopathy. We invite you to contact us with any questions or schedule an appointment today.


