Branch Vein Occlusion
What is a branch retinal vein occlusion?
A branch retinal vein occlusion (BRVO) is a problem of the retina that can cause blurred vision.
The retina lines the back wall of the eye. It is responsible for receiving light from the outside world and sending the light image to the brain. The retina needs nutrients and oxygen to survive, it receives these through a central retinal artery. When the retina is done feeding on nutrients and oxygen, the remainder is brought out of the eye by the central retinal vein. In order to drain all the areas of retina there are many venous branches that lead into the central vein. Some areas of veins and arteries overlap. The vein is softer than the artery so when the space they share gets tight (because of high blood pressure, high cholesterol or having thick blood) the vein collapses a clot forms and blood can no longer drain from the vein. This is known as a branch retinal vein occlusion and the problem arises when blood that should be draining backs up into the retina.

A color photograph of the retina showing a branch retinal vein occlusion with blood backed up into the retina in the area drained by the affected vein.
Learn more about branch retinal vein occlusion (BRVO) at ASRS
Información en español en el sitio web de ASRS
Who is at risk for having a branch retinal vein occlusion?
Patients with high blood pressure, high cholesterol, diabetes and more rare conditions that cause thick blood like multiple myeloma. Sometimes, patients develop BRVO without having risk factors.
What causes a branch retinal vein occlusion?
As the branch retinal vein collapses, blood flow slows down, more blood sticks to the wall of the vein -becoming a clot- and preventing blood from leaving the retina. The blood backs up into the retina filling the normally dry retina with fluid and expanding it like a sponge. A wet retina does not work normally and this causes vision to worsen. Sometimes blood backs up so much that there is no room for fresh blood carrying oxygen and nutrients. Without proper nutrients these areas of retina may die.
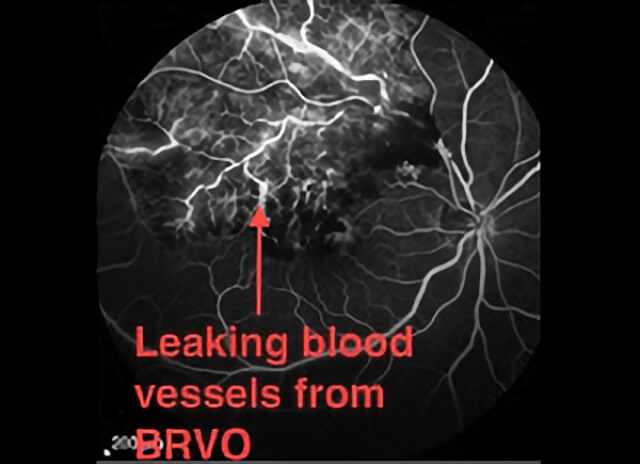
A fluorescein angiography photo showing a branch retinal vein occlusion with damaged blood vessels in the distribution of the affected vein.
How is a branch retinal vein occlusion diagnosed?
Usually someone notices blurry vision in one eye that can develop over one to several days. There can be a wide range in vision loss, from a subtle fogging of the vision, to severe vision loss where someone may only be able to appreciate a hand moving in front of their face. Sometimes a patient may go to their general eye doctor to see if new eyeglasses help, but this type of vision loss does not improve with glasses. Examination of the retina with specialized lights and lenses after dilation of the pupils can discover signs of BRVO. Computerized photographic tests such as a fluorescein angiogram (FA) and optical coherence tomography (OCT) help in evaluating the blood vessels and assessing the amount of fluid that has accumulated in the retina1 (Shah 2015). An FA is done by injecting an orange dye into a vein of the arm and taking special digital photographs of the dye as it flows through the blood vessels in the retina to look for abnormalities. An OCT is a painless computerized scan of the retina that provides a detailed view of the inner retinal structures.
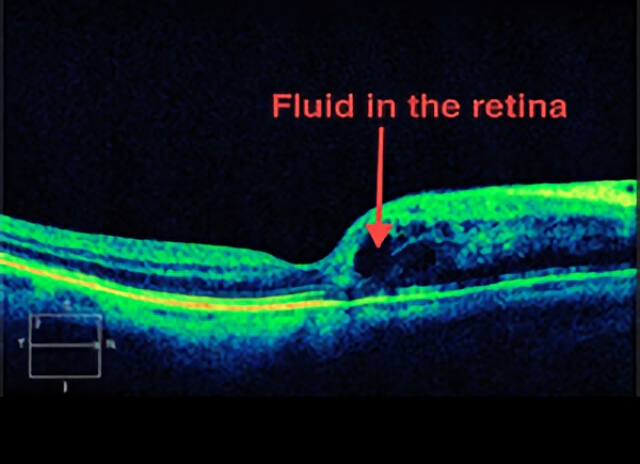
An OCT photograph of a macula with fluid accumulating in tiny retinal spaces as a result of a branch retinal vein occlusion.
What can be done for a branch retinal vein occlusion?
In areas of retina that have been damaged due to lack of nutrients and oxygen, laser can be applied to prevent further damage. Historically lasers have been used more frequently, but with the success of injectable steroids and anti-VEGFs, lasers have had a more secondary role. For vision that is reduced because of fluid accumulation, anti-VEGF and steroid medications can help fluid reabsorb. Anti-VEGF medications were developed to remove VEGF (Vascular Endothelial Growth Factor), a major factor in making blood vessels leaky. These medications must be delivered as an injection in the eye after anesthetic and antiseptic treatment to the eye to make the injection as comfortable and safe as possible. Since the introduction of anti-VEGF medications, many clinical trials have proven their efficacy2 (Ou et al. 2017). Results show that 2 out of 3 patients with fluid in the retina can have visual gains with monthly injections. Bevacizumab (Avastin), Ranibizumab (Lucentis), and Aflibercept (Eylea) are the most useful anti-VEGF drugs we have available today. Steroids help damaged blood vessels heal properly and a long acting dexamethasone steroid implant (Ozurdex) has been found to be helpful in improving vision. Your retinal consultant will help decide which medicine is right for you.
How frequently do I need Injections?
The anti-VEGF agents currently available last for 4-6 weeks before their effects fade and a new injection is typically needed. The steroid implants may last even longer. Most clinical trials show that treatment every 4-8 weeks gives the best results. Some patients need more frequent injections and others need less frequent injections. The intervals required by any one patient may change with time. Your doctor will decide with you how frequently you need treatment.
Does the injection hurt?
The procedure is quick and practically pain free for most patients. A sterile lid speculum helps keep the eye open and an antiseptic kills any germs. It is common for the eye to feel irritated and scratchy for a day after the injection. Worsening vision and severe pain, especially if it is not improving after the first day may be signs of an infection after an eye injection and if you have these symptoms you must contact your doctor.
Will I go blind from branch retinal vein occlusion?
There is a wide range in visual outcomes for patients with BRVO and the final visual outcome cannot be predicted. In general the worse the vision is after the initial insult, the worse the prognosis. In eyes where the nutrient and oxygen flow has been disrupted there is a higher likelihood of severe vision loss. Almost certainly the vision will not be the same compared to before the BRVO insult, however, more than half of patients can expect improvement in their vision with time.
References
- Shah AR. Widefield Imaging Finds Its Place in the Practice. Retina Specialist. November 2015; Accessed January 2022: retina-specialist.com/article/widefield-imaging-finds-its-place-in-the--practice
- Ou WC, Brown DM, Payne JF, Wykoff CC. Relationship Between Visual Acuity and Retinal Thickness During Anti-Vascular Endothelial Growth Factor Therapy for Retinal Diseases. Am J Ophthalmol. 2017 Aug;180:8-17. pubmed.ncbi.nlm.nih.gov/28549848
Schedule Branch Vein Occlusion Treatment in Northern California with Retinal Consultants Medical Group
Since 1975, Retinal Consultants Medical Group has been providing outstanding care to patients throughout Northern California, including Sacramento, Modesto, and Stockton. Our retina specialists and surgeons treat multiple vitreoretinal conditions, such as age-related macular degeneration and diabetic retinopathy. We invite you to contact us with any questions or schedule an appointment today.


